What is palliative care?
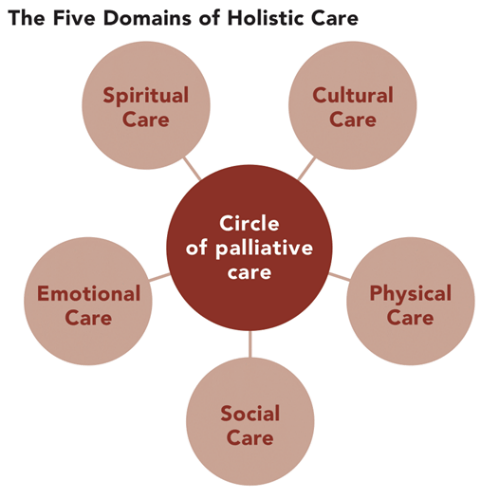
Palliative care is specialized medical care for people living with a serious illness. It is an approach that improves the quality of life of patients and their families who are facing challenges associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual. This type of care is focused on providing relief from the symptoms and stress of the illness. The goal is to improve the quality of life for both the patient and caregiver. This involves a range of services delivered by a range of professionals that all have equally important roles to play – including physicians, nurses, support workers, paramedics, pharmacists, physiotherapists and volunteers providing an extra layer of support. If willing, palliative care can work with the patient’s family as well.
According to the World Health Organization (WHO), each year, an estimated 40 million people are in need of palliative care; 78% of them are living in low and middle-income countries. Worldwide, only about 14% of people who need palliative care, are currently receiving it. The global need for palliative care will continue to grow as a result of the ageing of populations and the rising burden of non-communicable diseases and some communicable diseases.
To achieve the Sustainable Development Goal and work towards universal health coverage, countries have to strengthen palliative care services. WHO works with countries to include palliative care as a key part of their health systems. Adequate national policies, programmes, resources, and training on palliative care among health professionals are urgently needed in order to improve access and emphasis should be given to a primary health care approach.
Why is a basic understanding of palliative care essential?
In the past, palliative care was mostly provided to patients with a diagnosis of cancer. But for the time being, it is well recognized that everyone who is diagnosed with a life-limiting illness, including cancer, chronic diseases and end-stage organ failure and patients with end-stage and non-malignant diseases, for example, end-stage heart failure, renal failure and neurological conditions such as motor neuron disease, multiple sclerosis and dementia etc. may benefit from palliative care. As a caregiver, managing patients with one of these conditions, you should adopt a holistic approach that will ensure good, balanced medical care, whether this is in the patient’s last few years or days of life.
Does palliative care mean death?
Having palliative care doesn’t necessarily mean that the patient is likely to die soon – some patients receive palliative care for years. Patients can receive palliative care at any stage throughout their illness and alongside treatments; therapies and medicines are aimed at controlling your illness such as chemotherapy or radiotherapy including caring at the end of life. Some patients recover and move out of palliative care whereas others with chronic diseases such as COPD may move in and out of palliative care as the need arises.
Oftentimes, we hear people use the terms “palliative” and “end-of-life” care interchangeably. This forms the common misconception that palliative means certain death. While it encompasses end-of-life care or hospice care, palliative care is not only for people who are terminally ill.
Palliative care involves the treatment of individuals who have a serious illness in which a cure or complete reversal of the disease and its process is no longer possible, and end-of-life care is a portion of palliative care that is directed towards the care of persons who are nearing the end of life.
Both palliative and hospice care provide comfort. But palliative care can begin at diagnosis, and at the same time as treatment. Hospice care begins after treatment of the disease is stopped and when it is clear that the person is not going to survive the illness.
Both palliative and hospice care provide comfort. But palliative care can begin at diagnosis, and at the same time as treatment. Hospice care begins after treatment of the disease is stopped and when it is clear that the person is not going to survive the illness.
“There is an end to CURE: there is no end to CARE”
What are the stages of palliative care?
Palliative Care: Includes, prevention, early identification, comprehensive assessment, and management of physical issues, including pain and other distressing symptoms, psychological distress, spiritual distress, and social needs.
Can palliative care be done at home?
Palliative care services can be provided in a range of settings: including your home, an aged care home, hospital, or a palliative care unit. There are also specialised palliative care services to cater for diverse needs. Services that can be provided at home include:
- Personal care such as help with dressing, bathing and toileting
- Continence care
- Help with medication
- Pain management – both physical and emotional
- Help with mobility, including home adaptations to help you move around the house
- Housekeeping
- Preparation of meals
What are the benefits of palliative care?
- Puts the patient’s desires, goals and decisions first
- Supports the patient and family
- Helps patients and families understand treatment plans
- Improves quality of life
- Provides pain and symptom control
- Focuses on body, mind and spirit
- Reduces unnecessary hospital visits
What are the negative consequences of palliative care?
- commitment composed of adaptation and extra work and demands
- composed of frustration and uncertainty
- can often feel stressed and overwhelmed
‘We have added days to life; it’s time to add life to days.’
| By Dr Chamindu Raigamkorale, Dr Shanika Mututanthri |